Evidence in Action
"From HIV to Global Health Impact.”
About
Evoking collaboration and evidence-based impact across diseases


A future where lived experience drives innovation, strengthens accountability, and delivers lasting global health impact.
Mission
To leverage multi-sectoral partnerships and the lived expertise of people living with HIV to drive evidence-based advocacy, strengthen multi-disease integration, and promote equitable access to prevention, treatment, and care across Africa and the Global South.
Background
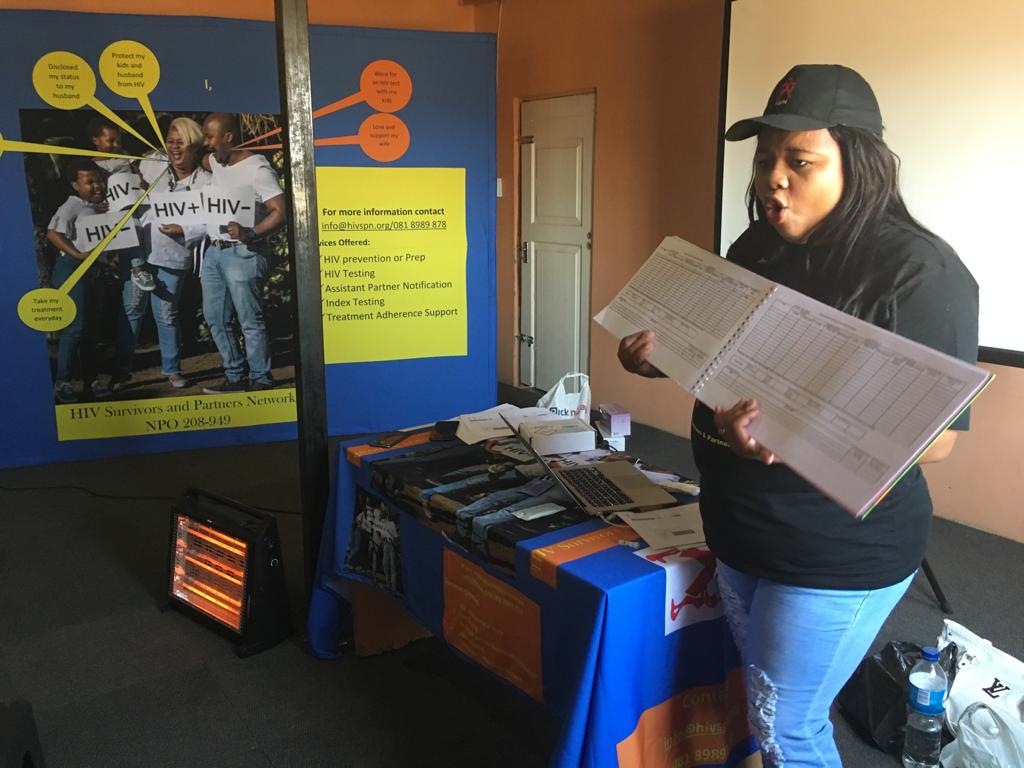
HIV Survivors and Partners Network, headquartered in South Africa and active across Africa, is a PLHIV-led organisation with over 20 years of lived experience and technical expertise in HIV prevention, treatment, and programme support. HSPN collaborates with organisations across Africa and co-founded U=U Africa Forum (a peer led organisation that seeks to advocate for adoption of U=U across the region) under the auspices of https://preventionaccess.com/
The organisation goals are to:
Advance Evidence-Driven and Integrated Health and Community Systems: Promote the use of real-world evidence, implementation science, and community insights to strengthen multi-disease, person-centred models of care across HIV, NCDs, STIs, and emerging public health threats.
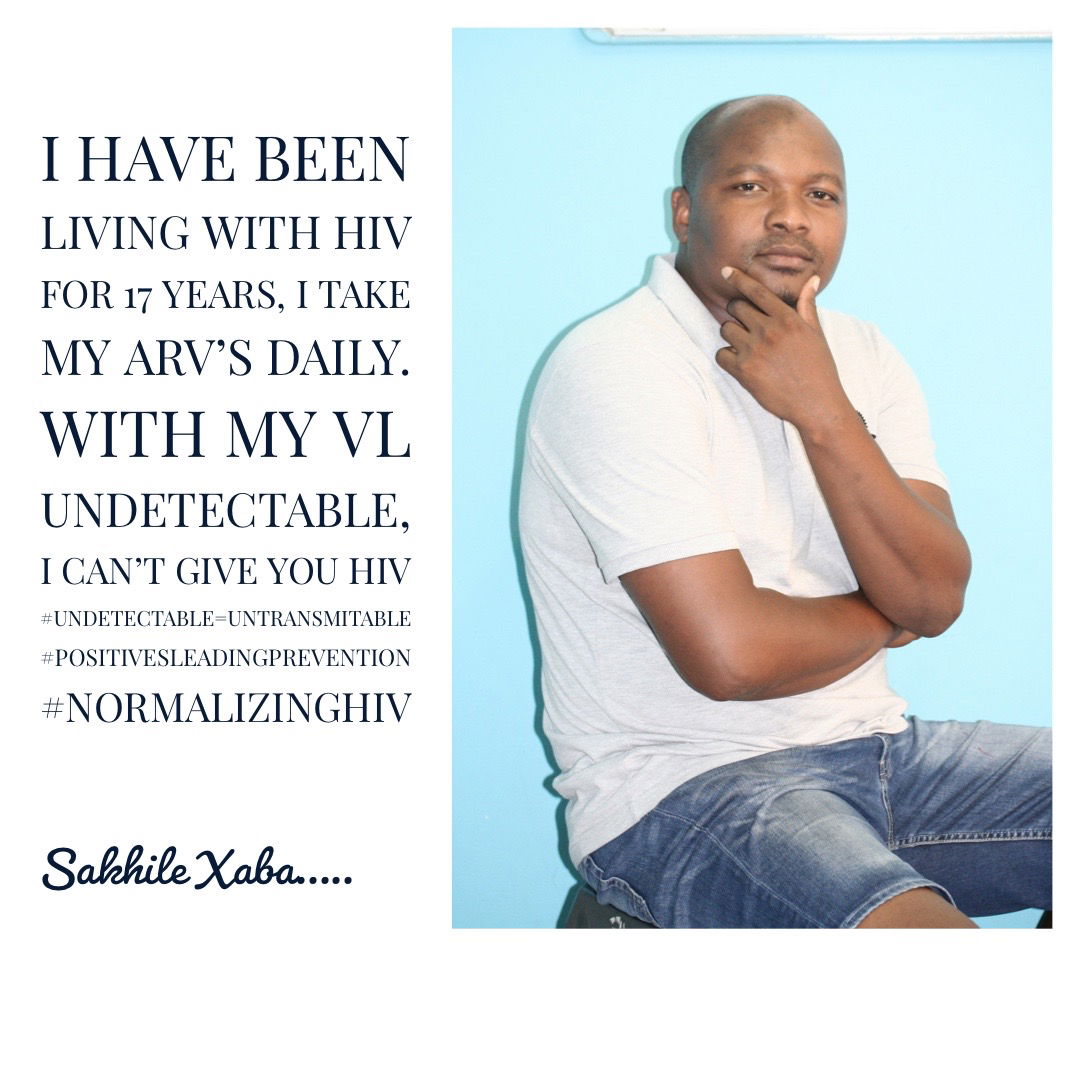
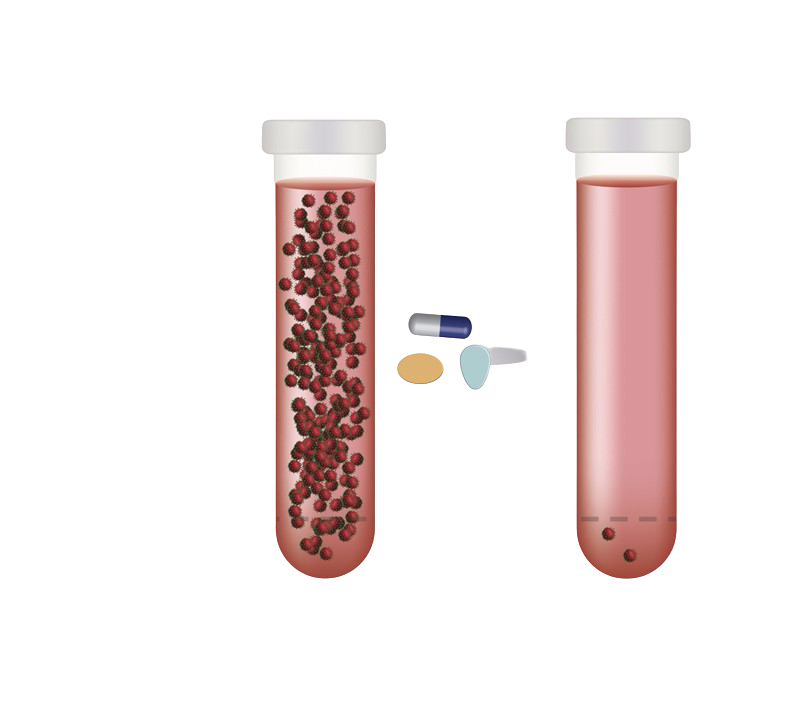
Leverage U=U to Accelerate the Ending AIDS Agenda: Use U=U as a transformative, evidence-based tool to reduce stigma, strengthen treatment outcomes, and expand equitable access to ART, and viral load monitoring as well as mobilising communities and decision-makers to fast track progress toward ending AIDS as a public health threat by 2030 and beyond.
Strengthen PLHIV Leadership & Community Power: Amplify the leadership, voice, and agency of people living with HIV in shaping policies, programmes, and innovations that sustain HIV treatment gains and advance broader global health priorities.
Ensure Equitable Access to Prevention, Diagnosis & Treatment: Advocate for fair, affordable, and sustainable access to essential diagnostics, medicines, technologies, and high-quality service, particularly for underserved populations in Africa and the Global South.
Team
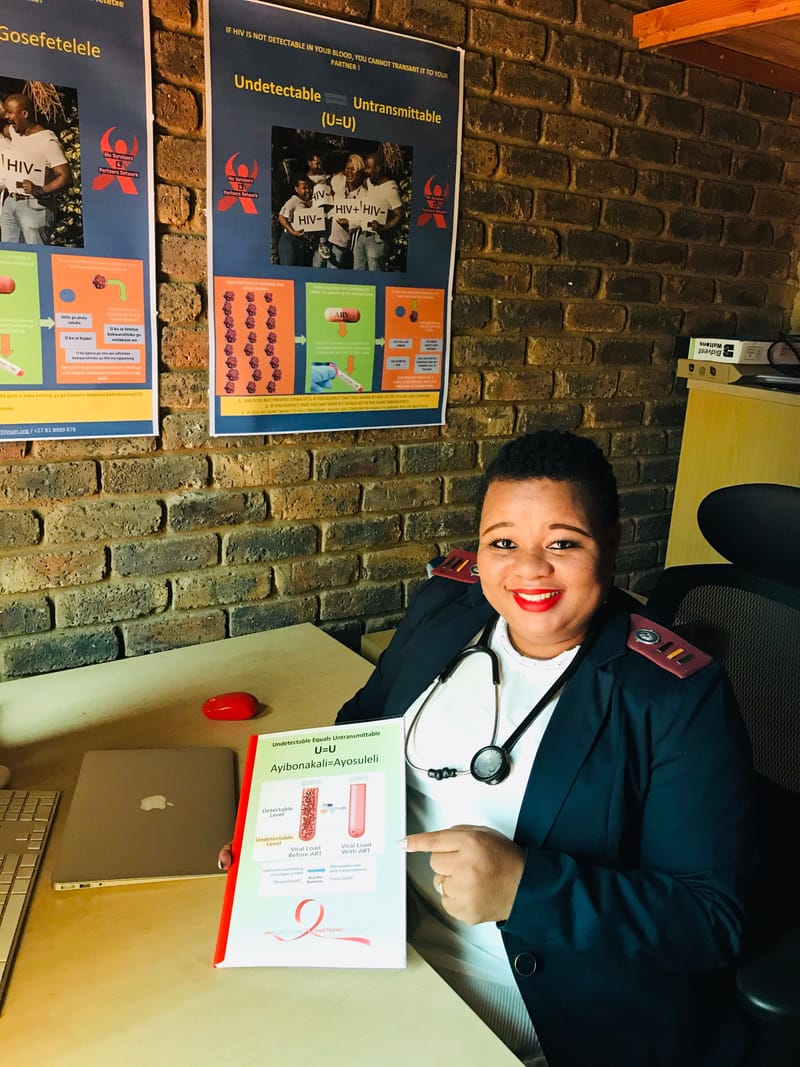
Angela Motsusi is a clinician with more than 10 years working in the clinical management of HIV and an HIV activist . She is a U=U pioneer in S.A and a co-founder of the organisation.
Angela Motsusi
Nomatamsanqa Nomlala a Xhosa woman who grew up in the famous province of Nelson Mandela who hails from the Eastern Cape. She holds qualifications in Logistics, Imports and Exports for developing countries coupled with a number of certificates in business. She has 20 years work experience working in different sectors whereby she has been responsible for driving business growth and stakeholder engagement. She has developed a network of contacts locally and internationally to attract new business, constantly researches new market opportunities and oversee growth of projects, making income projections and forecasting revenue. Motto: Health gives you the power to make wealth
Nomatamsanqa Namlala
Legae Sebakwane is an Omnichannel Strategist and Content Creator with experience in the media sector for over 21 years. He has been nominated for some of his work on national platforms in the creative industry and has consulted for various public sector and private organisations both locally and internationally. Also NGO's funded by AU, EU & UN have consulted him to do their reports for transparency and accountability. He has worked on Blockchain projects as a Chief Innovation Specialist and is a member of the African Circular Economy Network.
Mr Legae Sebakwane
Ms Khuthala Govana hold a Masters in Public Health Degree and Honours Bachelor of Arts (Social Behavior Studies in HIV/AIDS). She has vast experience in coordinating different HIV project and in developing programs and policies. She contributed a lot in scaling up Peer promotion propgram for Eastern cape universities. She was leading the development of curriculum for the peer educators program and its roll out plans. She is well experienced with developing work plans and monitoring tools.
Khuthala Govana
Services
Advancing Evidence-Driven Community and Health Systems

Co- Designed U=U South Africa Campaign
U=U workshops for HCW's and CHW's Demand Creation Community and Social Media Campaigns Radio and Television talks IEC Material Designing

Advocacy
Advocating for PLWHIV and CLHIV to equal access HIV services-

Safe Space for Women and Girls with HIV
Platform where girls and women with HIV receive real time and non-judgmental advise from nurses living with HIV

Community Systems Strengthening
Peer led Capacity Building for civil society, non governmental, government and private businesses.
HCW's in Aids Care Program
Training and Mentoring for HCW's in Aids Care Championing Patient Centered Care- Annual Conferences
Peer Led Direct Service Delivery
Tracking and Tracing disengaged clients Peer Led- Community Based HIV Testing/Index /Couple Testing Safer Conception Service Advise and Referral Prep/HAART distributors
Training Application form-HCW's in HIV Care
Employee Health and Wellness Service Request
Membership Registration
Consider that your organisation is registered with DSD/CIPC as a:
Faith-based organisation
Community-based organisation
Network of PLHIV
If you are a civil society organisation, we invite you to become a partner of HIV Survivors and Partners Network. Partnership is open to organisations working in the HIV sector as well as international networks and institutions active in the field of HIV/AIDS in South Africa and or Africa. Read more information about partnerships below.
Why become a member?
Membership enables you to get discounted:
Capacity Building opportunities (Training and Mentoring)
Equipment and tools required to deliver your HIV services
Peer led personalised IEC material with real life stories of PLWHIV for your campaigns
Demand creation campaigns
You also benefit from:
Exchange experiences with other NGO's
Present your concerns and priorities to key players at the Districts and National level
Join the Champions of Change virtual mentorship sessions
What does membership include?
As a member you will have access to:
regular e-newsletters on activities and forthcoming events
help in finding a partner for specific projects
resource material on our website
information in the Clearinghouse to share expertise and experiences
Commitment of members
We consider membership a two-way process. It enables you to share your best practices at the National and Regional level while at the same time you can learn from other experiences. Members contribute to and promote HSPN policies and programs in their countries. Membership means commitment for action.We welcome voluntary contributions, financial or in-kind, from members, as we depend on external support to enable the partnership to develop further.
Our partners are "first" and "second" sector organisations that are active in the field of HIV/AIDS in South Africa and/or Africa, including:
National and Regional networks
Governmental organisations
Global networks
International organisations
Universities
Private for profit organisations
Partnership enables you to:
Get more visibility with your partner profile on our website (to present your organisation and its work)
Having opportunities to connect to more than 400 civil society organisation in Africa
Referral hub for your clients to join HSPN peer led virtual support sessions
Opportunity to showcase your work on HSPN quarterly newsletter
If you represent a civil society organisation (non-governmental, faith-based, community-based, patient-based organisation or a professional association or national network) based in one of the African continent and active in the field of HIV/AIDS, you can register as a member of HSPN. Registered members will get a certificate endorsing the memberships with a unique code to use whenever they join sessions/request services
Join us
Champions of Change
Client Centred Care
Blog
PLWHIV are placing themselves at the centre to End the Epidemic by 2030
Leading STI Advocacy and Literacy: We are providing communities with the knowledge they need to make informed sexual health decisions, recognise symptoms, understand treatment options, and challenge stigma. By combining strong diagnostics, comprehensive prevention, and community-centered education, STI advocacy drives improved health outcomes, reduces transmission, and supports healthier, more empowered populations
Read MoreDespite widespread support for MIPA principles, meaningful involvement of PLHIV and other community stakeholders can be challenging to achieve and is not applied consistently in all areas of HIV-related clinical research. A recent systematic review found that community stakeholder involvement predominantly occurs in the early stages of a trial, often to support participant recruitment, but is limited in later trial stages. Methods used to engage with communities are also often researcher driven and utilize formal consultation methods, such as interviews or focus groups, that do not afford PLHIV any power to influence the research process. A team of close to 150 HIV Cure CAB members and Cure alumni's met to discuss strategies to ensure continuous meaning involvement of community in the Cure Agenda
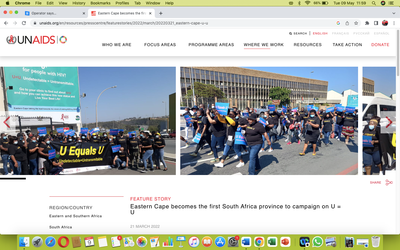
Read MoreEastern Cape becomes the first South Africa province to campaign on U = U. HSPN among the few organisations that initiated the concept and led the launch
Read MoreThis segment of serodiscordant couples (SDC) is aware of their discordance (that one of them has HIV and the other does not) and have had their relationship disrupted by it in some way. They may be experiencing blame over who brought HIV into the relationship, disconnection around sex, and/or discouragement around conceiving. The discordance has been so disruptive for some that they now face the “discordance dilemma.” They see the avoidance of HIV transmission at odds with preserving their relationship. Other couples endure the discordance out of love and commitment, but the risk of HIV transmission is still disruptive, complicating the things they want and value in their relationship—intimacy and children. For Serodiscordant partners enrolling in PrEP is often perceived as more burdensome than helpful. Bringing up PrEP may resurface undesirable, negative feelings associated with the discordance, such as blame, guilt, and even violence. In visiting an HIV clinic, SDC risk disclosing their discordance to others, and partners without HIV risk being mislabelled as HIV positive. And taking PrEP may bring on undesirable stigma from others. Thus, when SDC compare PrEP to other HIV-prevention tools like condoms, many struggles to be convinced of its relative effectiveness and appeal.
Read MoreContact us
Evidence in Action "From HIV to Global Health Impact.”
- Centurion, Gauteng, South Africa
- 0861201923
- programs@hivspn.org
- 08:30-16:30
If you want counselling about living positive with HIV, struggling with adherence, status discloser to your partner or information about safer conception please send us an email to schedule an appointment
Projects and Events
The congress will bring together researchers, policymakers, civil society, and industry leaders to translate cutting-edge HIV research into actionable policies and practices, strengthen evidence-based decision-making and promote innovative solutions to improve public health outcomes across Africa
Mandisa Dukashe- the founder of HSPN approached the E.C to secure a buy-in from the policy makers and leaders of the province. The campaign was finally and officially launched with pledges of support from Eastern Cape Premier Oscar Mabuyane, community members and other prominent stakeholders, including the Eastern Cape Provincial AIDS Council, the Department of Health, the South African National AIDS Council and UNAIDS. Eastern Cape was the first of nine provinces in South Africa to launch a public information campaign to raise awareness of U = U (undetectable = untransmittable) and to encourage people living with HIV to commence, maintain or resume treatment and achieve and maintain an undetectable viral load. For more information, please read here: https://www.unaids.org/en/resources/presscentre/featurestories/2022/march/20220321_eastern-cape-u-u
Conducted district based dialogues and engagements with various civil society organisation to promote the uptake of U=U messaging. Advocated for adoption and integration of U=U in demand creation programs to promote retention to care and distigmatise HIV. These engagements led to a wide and national adoption of U=U, and eventually a national launch (following various district based and provincial launches)
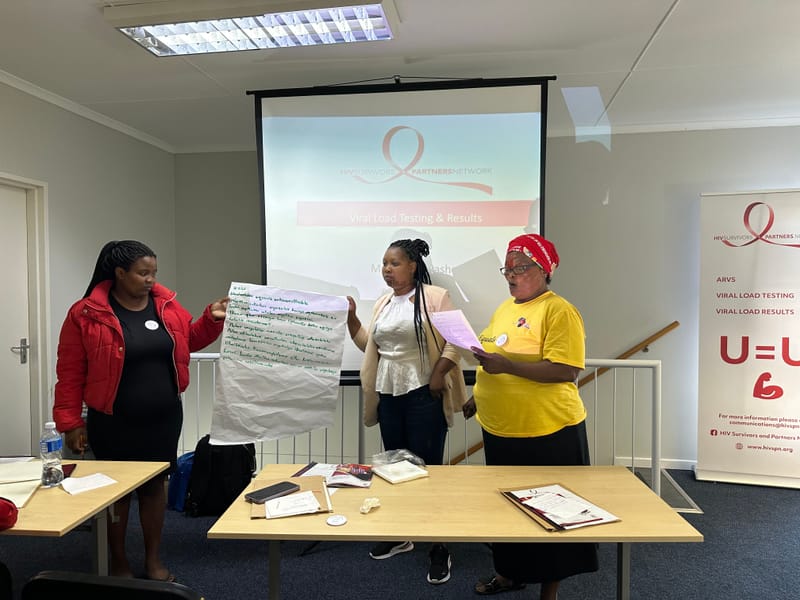
HSPN convened dialogues with organizations to 1) understand community perspectives on VL testing access and practise; 2) ensure community engagement in HIV monitoring research studies; and 3) generate broad- based community support and demand for innovation products and conducted a series of country-level landscape analyses on VLT to better understand the current context, assess barriers and facilitators to VLT among community members. HSPN worked with community stakeholders to co-create a community engagement plans and hosted five workshops on VLT access and education of approximately 20 attendees. At the conclusion of the fifth workshop, HSPN hosted a community advocacy in Johannesburg in relation to VLT access advocacy.
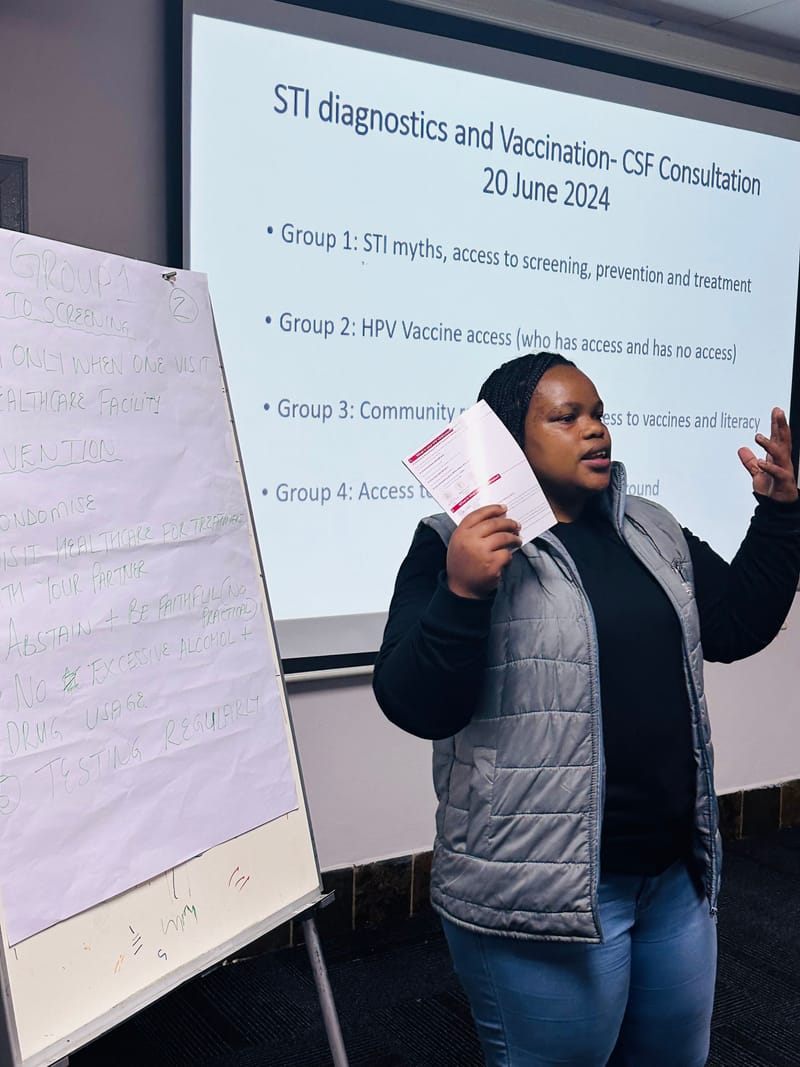
Through consultations with local government officials and civil society leaders in North West, Gauteng, and KwaZulu Natal Provinces, the HIV Survivor’s Partner Network identified several major STI prevention gaps. They found that test kit shortages lead providers to diagnose STIs based on symptoms alone, which may lead to under- or over-treatment and could potentially exacerbate antimicrobial resistance. They also noted that limited HPV vaccination coverage leaves significant populations, including adult women, boys, and girls who attend private schools, unprotected. Specifically, they found that only 35% of HIV testing clients were screened for STIs, and that many community organizations lacked STI literacy materials. Additionally, most private school girls had not been offered the free HPV vaccine, underscoring the urgent need for policy reforms. They call for greater civil society engagement to advance STI literacy and advocate for new diagnostics and vaccines.